On August 11, 2014, entertainment genius Robin Williams took his own life inside his Paradise Cay, California home near San Francisco. The coroner initially ruled that Williams, age 63, died by suicide—asphyxia by hanging antecedent to, or caused by, clinical depression. However, when the final autopsy results were in, an entirely different picture played out. Robin Williams was in the advanced stage of a somewhat common, but almost always undiagnosed, brain disease called Lewy Body Dementia or LBD.
On August 11, 2014, entertainment genius Robin Williams took his own life inside his Paradise Cay, California home near San Francisco. The coroner initially ruled that Williams, age 63, died by suicide—asphyxia by hanging antecedent to, or caused by, clinical depression. However, when the final autopsy results were in, an entirely different picture played out. Robin Williams was in the advanced stage of a somewhat common, but almost always undiagnosed, brain disease called Lewy Body Dementia or LBD.
As Williams’ window, Susan Schneider Williams who now represents the Lewy Body Dementia Association, stated, “The disease was a terrorist in my husband’s head. Any way you look at it, the presence of Lewy bodies in his brain took his life. Depression was only a symptom. Unfortunately, we as a culture don’t have the vocabulary to discuss brain disease in the way we do about depression. Depression is only a side effect of LBD—it’s rooted in neurology. His brain was literally falling apart, and not one thing could be done about it.”
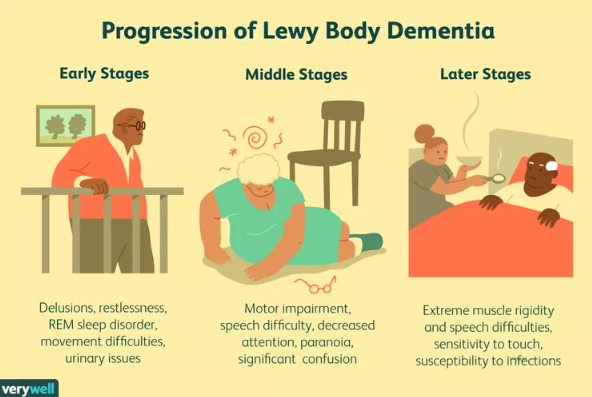
Lewy Body is a strange term. We’ll examine where that name came from, what exactly LBD is, what causes it, and how this always-fatal disease can be managed in its three progressive stages: early, mid, and late. But first, let’s have a brief look at this remarkable man’s achievements. Perhaps “remarkable” isn’t a powerful enough word for Robin Williams.
Robin McLaurin Williams was born on July 21, 1951, into an average American family. But from an early age, there was nothing average about him. He showed a God-given gift for improvision comedy and acting. By the early 1970s, Williams was in high demand as a San Francisco-based stand-up comedian, and he went on to be one of the funniest funnies of all time.
 Few can forget many of Robin Williams’ outstanding character roles. He got his television start in Mork & Mindy and went on to film. Popeye. Hook. Good Will Hunting. Dead Poets Society. Good Morning Vietnam. The World According to Garp. World’s Greatest Dad. Night at the Museum. The Birdcage. Moscow on the Hudson. Jumanji. And, of course, Mrs. Doubtfire.
Few can forget many of Robin Williams’ outstanding character roles. He got his television start in Mork & Mindy and went on to film. Popeye. Hook. Good Will Hunting. Dead Poets Society. Good Morning Vietnam. The World According to Garp. World’s Greatest Dad. Night at the Museum. The Birdcage. Moscow on the Hudson. Jumanji. And, of course, Mrs. Doubtfire.
Williams also did voice-overs in Aladdin, Robots, and Happy Feet. He won numerous awards—six Golden Globes, five Grammys, two Primetime Emmys, two Screen Actors Guilds, and an Oscar for Best Supporting Actor. As well, Williams won the Cecille B. DeMille award in 2005.
Robin Williams had his struggles through life, though. He was addicted to cocaine and alcohol which set him into fitful mood swings. He was in and out of rehab for years. However, by 2010 he was stable and substance free, except for therapeutic prescriptions issues to combat what was thought to be clinical depression.
It was not. Robin Williams had an undiagnosed brain disorder. A disease that was only discovered after his death and was verified by brain sectioning at his autopsy. What was suspected to be Alzheimer’s or Parkinson’s in the last year of his life turned out to be Lewy’s Body Dementia—a condition under the general dementia umbrella and an extremely deadly disease.
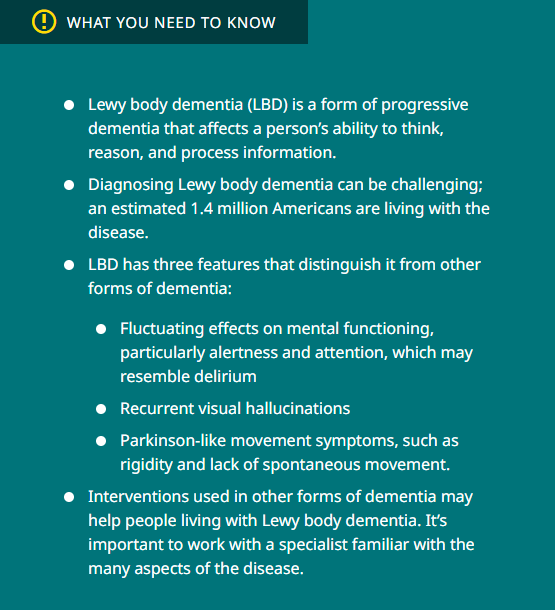
You’re likely wondering what this weird name is and what it entails. Rather than me paraphrasing the information, let’s go to the best source available. No, not Wikipedia or ChatGPT. It’s the website of the Lewy Body Dementia Association, and here’s what it says:
Lewy body dementia (LBD) is the 2nd most common type of progressive dementia after Alzheimer’s disease. The name comes from a discovery by Dr. Friedrich Lewy in the early 1900s of abnormal bodies or deposits of alpha-synuclein proteins in areas of the brain that can only be verified through an autopsy. These bodies alter the production of dopamine and acetylcholine that are vital neural transmitters.
LBD is not a rare disease. It affects more than a million people in the United States alone. Because LBD symptoms may closely resemble other, more commonly known disorders like Alzheimer’s and Parkinson’s disease, it is widely under-diagnosed.
LBD is an umbrella term for two related diagnoses:
- A person with dementia with Lewy bodies will develop dementia and other LBD symptoms, one of which may be changes in movement, like a tremor (parkinsonism).
- With the other form of LBD, people will present first with changes in movement, leading to a Parkinson’s disease diagnosis; over time many will develop dementia years later. This is diagnosed as Parkinson’s disease dementia.
As time passes, people with both diagnoses will develop very similar cognitive, physical, sleep, and behavioral symptoms. The earliest symptoms of dementia with Lewy bodies and Parkinson’s disease dementia are different, but both are due to the same underlying biological changes in the brain.
LBD is a multi-system disease and usually requires a comprehensive treatment approach with a collaborative team of physicians and other health care professionals like occupational, physical, or speech therapists. Early diagnosis and treatment may extend your quality of life and independence. Many people with LBD enjoy significant lifestyle improvement with a comprehensive treatment approach, and some may even experience little change from year to year.
For a more in-depth explanation of Lewy Body Dementia disease, here’s a trip to the medical research department at Johns Hopkins University:
Lewy Body Disease (LBD) is a complex and often misunderstood neurodegenerative disorder that affects millions of individuals worldwide. Characterized by the accumulation of abnormal protein deposits called Lewy bodies in the brain, LBD poses significant challenges to both patients and caregivers. In this article, we delve into the neurological aspects of LBD, exploring its development, detection, effects on the human body, and its associated symptoms.
Development of Lewy Body Disease
Lewy Body Disease primarily affects older adults, typically manifesting after the age of 50. While the exact cause of LBD remains unknown, researchers believe that a combination of genetic, environmental, and lifestyle factors may contribute to its development. Genetic mutations, particularly in genes associated with the production and clearance of alpha-synuclein protein, have been implicated in some cases of familial LBD. However, most cases of LBD occur sporadically without a clear genetic link.
Neurological Pathology
At the core of LBD pathology is the abnormal accumulation of alpha-synuclein protein, forming Lewy bodies within neurons. These protein aggregates disrupt normal cellular function and communication within the brain, leading to widespread neurodegeneration. Areas of the brain particularly affected by Lewy bodies include the substantia nigra, which plays a crucial role in movement control, and the cerebral cortex, responsible for cognitive functions.
Detection and Diagnosis
Diagnosing LBD can be challenging due to its overlapping symptoms with other neurodegenerative disorders such as Parkinson’s disease and Alzheimer’s disease. A comprehensive medical history, neurological examination, and a battery of neuropsychological tests are often employed to assess cognitive function, motor abilities, and psychiatric symptoms.
Brain imaging techniques, such as MRI and PET scans, may reveal characteristic patterns of brain atrophy and dysfunction associated with LBD. Additionally, a definitive diagnosis of LBD can only be made post-mortem through the examination of brain tissue for the presence of Lewy bodies.
Effects on the Human Body
Lewy Body Disease has profound effects on both motor and non-motor functions, significantly impacting quality of life. Motor symptoms include bradykinesia (slowed movements), rigidity, tremors, and gait disturbances resembling those seen in Parkinson’s disease. Non-motor symptoms encompass cognitive impairment, hallucinations, fluctuations in attention and alertness, sleep disturbances, autonomic dysfunction (such as orthostatic hypotension and urinary incontinence), and psychiatric manifestations like depression and anxiety.
Treatment and Management
While there is no cure for Lewy Body Disease, various treatment strategies aim to alleviate symptoms and improve patients’ quality of life. Medications targeting dopamine levels in the brain, such as levodopa, may help alleviate motor symptoms. Cholinesterase inhibitors, commonly used in Alzheimer’s disease, may improve cognitive function and psychiatric symptoms in some LBD patients. Multidisciplinary approaches involving physical therapy, occupational therapy, speech therapy, and psychological support are essential for managing the diverse array of symptoms associated with LBD.
Takeaway
Lewy Body Disease presents a complex clinical picture characterized by the interplay of motor, cognitive, and psychiatric symptoms. Understanding its neurological underpinnings is crucial for early detection, accurate diagnosis, and effective management of the disease. Ongoing research efforts aimed at unraveling the molecular mechanisms underlying LBD pathogenesis hold promise for the development of targeted therapies that can ultimately improve outcomes for individuals living with this challenging condition.
I’ll jump back to the Lewy Body Dementia Association for the diagnostic symptoms of the disease.
Motor Symptoms
- Bradykinesia (slowed movements)
- Rigidity (stiffness)
- Tremors (usually less prominent than in Parkinson’s disease)
- Gait disturbances (shuffling gait, balance problems)
Cognitive Symptoms
- Fluctuating attention and alertness
- Memory loss
- Executive dysfunction (problems with planning, organizing, and problem-solving)
- Visuospatial difficulties (problems with spatial awareness and perception)
Psychiatric Symptoms
- Hallucinations (visual hallucinations are particularly common)
- Delusions (often related to the hallucinations)
- Depression
- Anxiety
- Apathy
- Irritability or aggression
- Sleep disturbances (REM sleep behavior disorder, vivid dreams, acting out dreams)
Autonomic Dysfunction
- Orthostatic hypotension (drop in blood pressure upon standing)
- Urinary incontinence or urgency
- Constipation
- Erectile dysfunction (in men)
Other Symptoms
- REM sleep behavior disorder (acting out dreams physically)
- Sensitivity to neuroleptic medications (may worsen symptoms)
- Changes in sense of smell
- Difficulty swallowing (dysphagia)
Note that not all individuals with LBD will experience all of these symptoms, and the severity and combination of symptoms can vary widely from person to person. Additionally, symptoms may fluctuate over time, with periods of relative stability interspersed with episodes of worsening symptoms. Early recognition and management of these symptoms are crucial for improving the quality of life for individuals living with LBD.
Detecting and verifying Lewy Body Disease (LBD) involves a comprehensive approach that combines clinical evaluation, neurological assessments, and diagnostic tests. Here’s a breakdown of the steps involved in the detection and verification process.
Clinical Evaluation
- A thorough medical history is obtained from the patient and their caregivers, focusing on the onset and progression of symptoms.
- A neurological examination is conducted to assess motor function, cognitive abilities, and psychiatric symptoms. This may include assessing gait, muscle tone, reflexes, coordination, memory, attention, and mood.
- Careful observation of symptom patterns, including fluctuations in cognition and alertness, visual hallucinations, and motor symptoms resembling Parkinson’s disease.
Diagnostic Criteria
- LBD is diagnosed based on established clinical criteria, such as the consensus criteria proposed by the DLB Consortium or the McKeith criteria.
- These criteria outline the characteristic features and diagnostic markers of LBD, including cognitive fluctuations, visual hallucinations, Parkinsonism, and rapid eye movement (REM) sleep behavior disorder.
- Criteria may also specify supportive features, such as neuroimaging findings and autonomic dysfunction, which further support the diagnosis of LBD.
Neuropsychological Assessment
- Neuropsychological tests are administered to evaluate cognitive function, including memory, attention, executive function, and visuospatial abilities.
- These tests help quantify cognitive impairment and track changes over time.
Neuroimaging Studies
- Magnetic resonance imaging (MRI) and positron emission tomography (PET) scans may be performed to assess brain structure and function.
- MRI may reveal patterns of cortical atrophy and changes in brain volume associated with LBD.
- PET imaging with radiotracers targeting dopamine transporters or amyloid plaques can provide additional evidence supporting the diagnosis and differentiate LBD from other neurodegenerative disorders like Alzheimer’s disease.
Cerebrospinal Fluid Analysis
- Lumbar puncture may be performed to analyze cerebrospinal fluid (CSF) biomarkers associated with LBD, such as levels of alpha-synuclein protein and markers of neuroinflammation.
- While not routinely performed, CSF analysis can provide supplementary information to support the diagnosis of LBD in some cases.
Genetic Testing
- Genetic testing may be considered in cases of familial LBD or when there is a strong family history of neurodegenerative diseases.
- However, genetic testing is not typically performed as part of routine diagnostic evaluation for sporadic LBD.
Multidisciplinary Evaluation
- A multidisciplinary team approach involving neurologists, neuropsychologists, geriatricians, psychiatrists, and other healthcare professionals is often utilized to ensure a comprehensive assessment and accurate diagnosis of LBD.
- Verification of LBD relies on the integration of clinical findings, diagnostic tests, and adherence to established diagnostic criteria.
- Given the complexity and variability of LBD presentation, accurate diagnosis and ongoing monitoring are essential for effective management and supportive care.
Treatment Options
- LBD is a multi-system disease and typically requires a comprehensive treatment approach, meaning a team of physicians from different specialties, who collaborate to provide optimum treatment of each symptom without worsening other LBD symptoms.
- A comprehensive treatment plan may involve medications, physical, occupational, speech or other types of therapy, and counseling.
Medications
- There are many treatments that can help with the symptoms; all medications prescribed for LBD are approved by the Food and Drug Administration to treat symptoms in other diseases, like Alzheimer’s disease and Parkinson’s disease.
- These medications can offer symptomatic benefits for cognitive, movement, sleep, mood and behavioral changes in LBD.
- There are not yet any medications that slow or stop the progression of LBD.
Cognitive Symptoms
- Medications called cholinesterase inhibitors are considered the standard treatment for cognitive symptoms in LBD.
- These medications were developed to treat Alzheimer’s disease. However, some researchers believe that people with LBD may be even more responsive to these types of medications than those with Alzheimer’s.
- These drugs sometimes help control behavior problems and hallucinations as well.
- Another medication that may be helpful is memantine (Namenda).
Movement Symptoms
- Movement symptoms may be treated with a Parkinson’s medication called carbidopa/levodopa (Sinemet), but if the symptoms are mild, it may be best to not treat them in order to avoid potential medication side effects.
Visual Hallucinations
- If the hallucinations are not disruptive, they may not need to be treated. However, if they are frightening or create challenging behavioral changes, a physician may recommend treatment.
- Cholinesterase inhibitors are sometimes effective in treating hallucinations and other psychiatric symptoms of LBD. In addition, newer ‘atypical’ antipsychotic medications may be tried.
- Most LBD experts prefer quetiapine or clozapine when treatment is necessary for safety or quality of life concerns.
- Caution is required to find the lowest effective dose in this situation.
- A newer medication, pimavanserin, was approved to treat psychosis in Parkinson’s disease; results from another clinical trial of this medication in people with dementia and psychosis are pending.
- While older ‘traditional’ antipsychotic medications such as thorazine and haloperidol are commonly prescribed for Alzheimer’s patients with disruptive behavior, these medications may cause severe side effects in those with LBD.
- For this reason, older traditional antipsychotic medications like haloperidol should be avoided.
WARNING: Up to 50% of LBD patients treated with any antipsychotic medication may have a severe reaction, such as worsening confusion, heavy sedation, and increased or possibly irreversible parkinsonism. If severe fever or muscle rigidity occurs, contact your doctor immediately; you may have a potentially life-threatening condition that is treated by stopping the medication.
REM Sleep Behavior Disorder (RBD)
- RBD can be quite responsive to treatment, so your physician may recommend a medication like melatonin and/or clonazepam.
Medication Side Effects
- Speak with your doctor about possible side effects.
- The following drugs may cause sedation, motor impairment, or confusion:
- Benzodiazepines, tranquilizers like diazepam and lorazepam
- Anticholinergics (antispasmodics), such as oxybutynin and glycopyrrolate
- Older antidepressants
- Certain over-the-counter medications, including diphenhydramine and dimenhydrinate.
- Some medications, like anticholinergics, amantadine, and dopamine agonists, which help relieve parkinsonian symptoms, might increase confusion, delusions, or hallucinations.
Surgery and Anesthesia
- Be sure to meet with your anesthesiologist in advance of any surgery to discuss medication sensitivities and risks unique to LBD.
- People with LBD often respond to certain anesthetics and surgery with acute states of confusion or delirium and may have a sudden significant drop in functional abilities, which may or may not be permanent.
- Possible alternatives to general anesthesia include a spinal or regional block. These methods are less likely to result in postoperative confusion.
- If you are told to stop taking all medications prior to surgery, consult with your doctor to develop a plan for careful withdrawal.
Other Types of Treatments
- Lifestyle interventions include eating a healthy diet, exercising, and remaining socially active.
- Physical therapy includes cardiovascular, strengthening and flexibility exercises, as well as gait training.
- Speech therapy may improve low voice volume, poor enunciation, muscular strength, and swallowing difficulties.
- Occupational therapy helps maintain skills and promotes functional ability and independence.
- Music and aromatherapy may reduce anxiety and improve mood.
- Individual and family psychotherapy may be useful for learning strategies to manage emotional and behavioral symptoms and to help make plans that address individual and family concerns about the future.
- Support groups may be helpful for caregivers and persons with LBD to identify practical solutions to day-to-day frustrations and to obtain emotional support from others.